What does a nose job have to do with a CFD simulation?
About 20 years ago, I myself underwent a nose operation at the German Armed Forces Hospital in Ulm because I had trouble breathing on one side of my nose.
Since I like to know what is happening, I followed the whole thing during the partial anesthesia. The surgeon acted like a sculptor with a hammer and chisel. As he did so, I wondered if he was working on the right areas and what would happen if he slipped. It is not one of my fondest memories, yet the subject has continued to occupy me. To what extent these medieval methods have perhaps given way to more modern procedures, I don't know, but whether the bone is removed in the right place is something we can tell you or the surgeon today with the help of flow simulations.
At that time, we had very long calculation times for simple flow models and the modeling effort was also extremely lengthy compared to today.
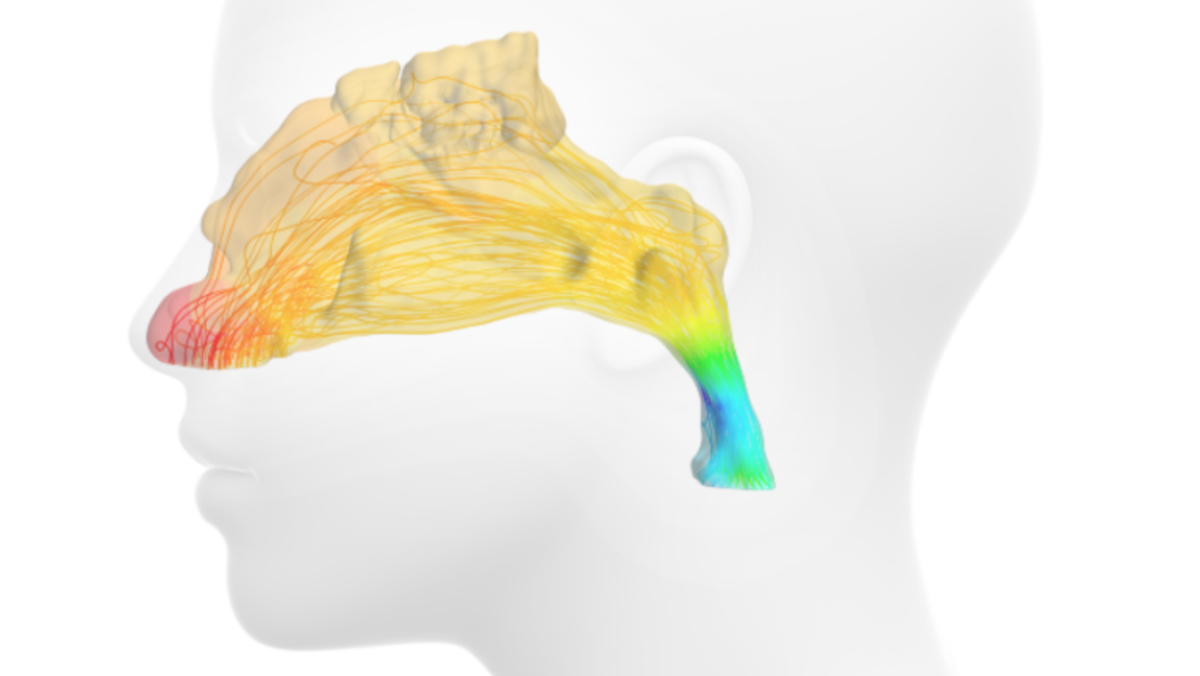
A flow calculation would have been difficult to impossible here, and the acquisition of the geometry and thus a CFD simulation would probably have been more the domain of a pathologist. Today, with little effort, we can use a CT scan to remodel the exact geometry of the bone and cartilage structure of the respective patient and determine the pressure loss or the volume flow of the two nostrils with a CFD simulation. Figure 2 shows the pressure curve, Figure 3 the streamlines.
By locally changing the nasal structure, the effects of a surgical procedure (expansion of the nasal space in the computational model) can be simulated.
The criterion whether the flow behavior becomes better or worse during surgery can be evaluated by clear numbers like the volume flow through the two nostrils at the same differential pressures.
In addition, CFD simulation can also be used to determine and evaluate the distribution of water vapor in the air we breathe. If we breathe in dry air, the lungs do not tolerate it so well. The air we breathe must be humidified. Here, the nose functions like an air conditioner, setting the right humidity. Figure 4 shows the dry air (blue) in the right nostril being drawn in and then humidified (red) going toward the trachea.
Perhaps in a few years it will be possible to simulate snoring by means of coupled structure and flow simulation (FSI=Fluid-Structure-Interaction).
Surgical procedures that provide relief would then be conceivable.
In any case, we are continuing to work on this topic at full speed.
With this in mind, I wish you staying power.
If you are wondering whether a CFD simulation is also possible for your own personal project, we will be happy to advise you. Please use our contact form.
Your Stefan Merkle